Gretchen L. Birbeck, E Chomba, […], and the Neurologic & Psychiatric Society of Zambia (NPSZ)
Additional article information
Background
Electroenphalograph (EEG) technology via a Natus Bio-Logic Ceegraph digital EEG machine will be available at University Teaching Hospital (UTH) very soon. In anticipation of this newly available technology, members of the Neurologic & Psychiatric Society of Zambia discussed the importance of optimizing the use of EEG. These guidelines have been developed with the recognition that EEG has the potential to substantially improve the care of select patients who are referred for an EEG study. Importantly, such improvements in care are only possible if the patients who receive EEG are appropriately selected for study and the recordings and interpretations are of sufficient quality.
The goal of these guidelines is to offer the referring and/or requesting clinician information on how to best select patients for EEG based upon existing evidence and guidelines from authoritative bodies in countries or regions where EEG is broadly available. Given the limited nature of the resource (only one EEG machine which could at the very most provide 5-10 EEGs per day), these guidelines will also try and offer priorities delineating where the use of EEG is likely to provide the greatest positive impact on patient care since prioritization may be required. Prior studies in multiple settings have established that at least a third of patients referred for EEG are referred inappropriately, meaning the study is very unlikely to offer information of value in caring for the patient [1-3]. Given the limited nature of the EEG resource, it is critical that inappropriate referrals be avoided. This NPSZ Advisory will also offer recommendations on training needs for optimal interpretation. It is important to recognize that inadequate training among persons interpreting EEG is most likely to result in “over interpretation” in which normal variants are interpreted as representing abnormalities that require treatment [4].
Methods
A comprehensive search without language limitations was completing using “EEG” OR “electroencephalography” with the limitation of “guideline” [5] in Pub Med from 1994 to 2010. Abstracts were reviewed and full-content of the articles were reviewed where the information seemed applicable to our search for guidelines on the conduct and use of EEG in the inpatient or outpatient settings. Guidelines for other technologies (e.g. evoked potential, continuous EEG monitoring) or settings (e.g. intra-operative monitoring) were excluded. Where an authoritative body developed multiple guidelines for the conduct of EEG over the study period, only the most recent guideline was retrieved. Information delineating strong clinical indications for EEG were abstracted and provided in evidence tables. This information was then placed in the Zambian/UTH context to develop formal recommendations (guidelines).
Results
Eighty-nine articles were identified. Many reports repeatedly emphasized the importance of recognizing that epilepsy is a clinical diagnosis and that EEG is not required for making the diagnosis or initiating treatment. EEG offers significant value in several settings. See Table 1. There is also clear evidence to indicate that EEG is not indicated in several clinical settings. See Table 2.
table ft1table-wrap mode=article t1
Table 1
caption a4
Indications for EEG
table ft1table-wrap mode=article t1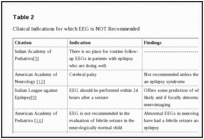
Table 2
caption a4
Clinical Indications for which EEG is NOT Recommended
NPSZ Recommendations
Indications for EEG
1 list-behavior=enumerated prefix-word= mark-type=decimal
2 Epilepsy–the propensity for recurrent, unprovoked seizures is a clinical diagnosis made based upon history-taking from the patient, family and/or other observer of suspected events. The physical examination may further support or refute the diagnosis of epilepsy. EEG is not required to make a diagnosis of epilepsy and treatment can and should be initiated without EEG in patients who are experiencing recurrent, unprovoked seizures.
3 An urgent EEG is indicated in all unconscious patients suspected of non-convulsive status epilepticus or subclinical seizures. This includes comatose or obtunded inpatients of unclear etiology especially those in whom seizures preceded the onset of coma.
4 While EEGs obtained after a first unprovoked seizure might offer insights into recurrence risk and/or the need for further neuroimaging, insufficient EEG resources are presently available to offer this service.
5 In children or adults with epilepsy which fails to respond to standard treatments and/or seizures and progressive neurologic problems, EEG may be warranted but this should be obtained through a neurologic consultation since such a consultation is needed to fully evaluate and assess such patients.
Quality Recordings
To assure an acceptable quality of EEG recordings, the technician(s) should receive training by skilled technicians using standardized montages [20-24] and following the recommended minimal technical requirements for performing clinical EEG[25-27]. Ideally, such training would occur in an environment as similar to UTH's as possible. Inquiries have successfully identified laboratories in Malawi and Uganda where a Zambian technician could receive training. Minimal requirements include at least 21 channels in the 10-20 International System or modified 10-20 system and records must be of at least 25 minutes duration. Brief outpatient records providing only 8 channels and/or only 5-6 minutes of recording are insufficient for assisting in the evaluation of a seizure disorder and are not recommended.
Quality Interpretation
To optimize EEG interpretation, opportunities for refresher training sessions in EEG interpretation are needed for UTH clinicians who have previously received training in EEG but who have not utilized the skill recently. UTH post graduates, primarily those in Paediatrics and Internal Medicine, would also benefit from training in EEG interpretation. Such training could be formal EEG educational courses offered through annual meetings held by neurological societies in Europe, the US and the UK as well as meetings held less frequently in South Africa. In addition to international training opportunities, EEG interpretation can also be optimized by offering onsite training at UTH. Onsite training opportunities will be made available in 2011. Any training provided will be developed to assist the trainee in adhering to recommendations for the optimal production of EEG reports [28, 29].
Quick Reference Summary Table
1 list-behavior=enumerated prefix-word= mark-type=decimal
2 EEG is not necessary for the diagnosis of epilepsy. If a patient is experiencing recurrent seizures, treatment should be initiated. Treatment should not be delayed to obtain an EEG.
3 EEG only provides information about what the brain is doing at the time of the recording. This means that EEG recordings may be completely normal, even in people who have epilepsy.
4 Sometimes people without epilepsy can have abnormal EEGs. This is especially true for people with migraine headaches and/or certain psychiatric disorders. An abnormal EEG must be considered in the clinical context and should not be reviewed in isolation.
5 EEG utilization at UTH will prioritize inpatients with possible subclinical seizures or nonconvulsive status epilepticus.
6 People with seizures that fail to respond to standard treatments and/or individuals with seizure disorders plus progressive neurologic problems should be referred for a full neurologic assessment, not just an EEG. Outpatient EEG referrals will be made by the specialist who sees the patient, if an EEG is determined to be needed.
7 A sufficient quantity of the prescribed medication should be provided to last until the patients next scheduled review date. Requiring patients to return more frequently than is necessary for collection of medications reduces adherence and adds additional barriers to care-seeking
Acknowledgements
Support for bringing EEG technology to UTH as well as development of these guidelines has been provided by The World Federation of Neurology (WFN), The World Neurology Foundation (WNF) and the US NIH 1R01NS061693-03S1.
Appendices
/article/back/app-group/app/
1. UTH Outpatient EEG/Neurology Referral Form
2. UTH Inpatient EEG Request Form

neuropsychiatry,epileptology, pulmonology and beyond.










